In my experience working with complex, chronically ill patients, some of the most challenging cases are those involving chronic infections.
Patients who’ve dealt with Lyme or Candida for years have often tried every supplement, prescription, and restrictive diet under the sun, yet are still living with debilitating symptoms. In some cases, the treatments have created a secondary set of problems by depleting patients’ microbiomes and nutrient levels.
This week, we’ll look at why these cases are so challenging, what the standard approach overlooks, and an alternative therapy to consider.
When an Infection Isn’t Really an Infection
One reason many patients struggle with “chronic infections” is because their treatment doesn’t target the underlying cause of their symptoms. In order to properly address the issue, we must differentiate between an infection and an immune-mediated response.
Active Infection
In an active infection, a pathogen is present where it doesn’t belong and your immune system attacks to neutralize the threat. An antimicrobial treatment, such as antibiotics or antivirals, eradicates the infection and the immune response stops.
Take acute Lyme disease for example. The Borrelia burgdorferi bacteria infiltrate your body via tick bite, which causes fever, headache, fatigue, and possibly a rash. If you’re lucky, you are diagnosed quickly, take antibiotics, and your symptoms subside.
Immune-Mediated Responses
An immune-mediated response develops when your immune system gets trigger happy and attacks when there is no real threat present. This occurs because you have lost tolerance to a substance within your body. It may be a virus, bacteria, or fungi that should be tolerated in small amounts, but your immune system still flags it as a threat. Or, it may be that the pathogen looks very similar to a tissue in your body, so your immune system goes after the tissue even though the infection has passed. The problem isn’t necessarily the pathogen, but how your immune system reacts to it.
In this scenario, you are bitten by a tick, the Borrelia burgdorferi bacteria trigger Lyme disease, and your immune system mounts an aggressive attack. Your immune system sends in wave after wave of inflammation to fight off the infection. This leads to inflammatory symptoms, such as arthritis, debilitating fatigue, numbness or tingling, declining brain function, or heart issues. You take stronger antibiotics that finally kill off the bacteria to non-symptomatic levels, but your immune system misses the memo and remains switched “on”.
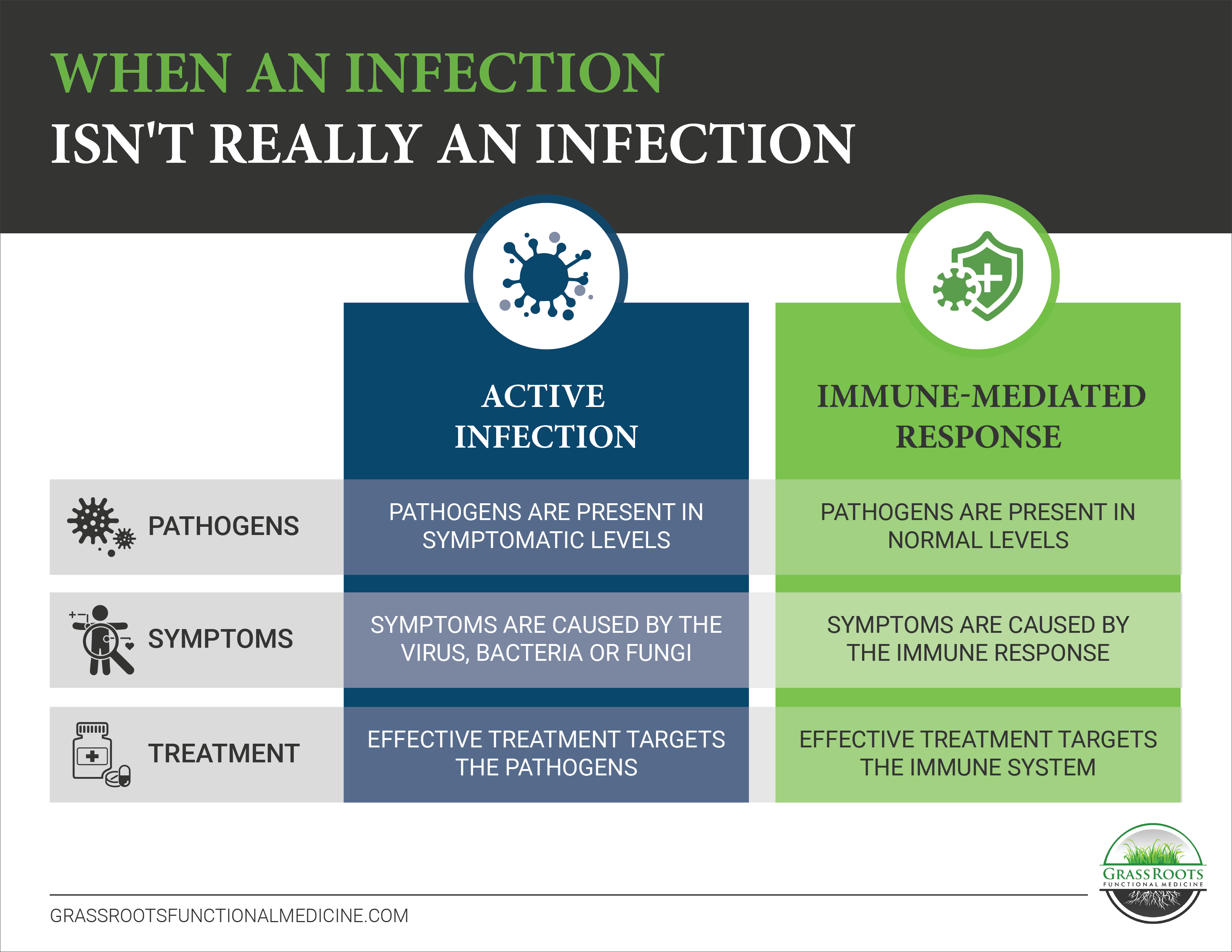
If you’re dealing with an immune-mediated response, you can keep treating the infection over and over again, but the symptoms either never stop or they come right back. In these instances, we must address the immune system itself to restore tolerance and support normal function.
How LDI Helps Stop the Immune-Mediated Response Cycle
Low-dose immunotherapy or LDI is designed to retrain your regulatory T cells so your immune system responds appropriately.
Patients are administered extremely low levels of biologically inert pathogens or allergens to slowly build up tolerance to their immune triggers. The concept is similar to allergy shots, but the concentrations are much lower and broader in scope.
In the case of chronic Lyme, patients are given extremely diluted doses of Borrelia burgdorferi and 74 common bacterial co-infections. The broad range of pathogens is key since many patients are dealing with a combination of these infections or may develop a reaction to them over time. Once patients reach their therapeutically correct dose (more on this below), their immune system switches “off” and the inflammatory symptoms subside.
Unlike traditional Lyme treatments like antibiotics and steroids, LDI treatments do not deplete the microbiome or immune system, and unlike allergy shots, it’s very rare to see a dramatic flare in symptoms.
What Infections Can LDI Help Treat?
Low-dose immunotherapy can be a helpful tool for:
- Lyme and co-infections
- Recurrent Candida overgrowth
- Parasites
- PANS and PANDAS
- Herpes
How Are Low-Dose Immunotherapy Treatments Given?
The antigen doses are given sublingually (under the tongue) every seven to eight weeks, in personalized concentration levels.
For treatment to be successful, you must determine your core dose – the specific antigen combination and concentration that relieves your symptoms. This is different for each individual and requires a bit of trial and error through the dose titration process.
During this process, the patient begins with a really low concentration and moves through progressively stronger doses every few days until they observe a response.
- If the dose is too low, you won’t see any response at all.
- If the dose is too high, you’ll see a temporary flare up in symptoms (typically mild to moderate). This indicates the antigen is correct and the titration simply needs to be refined.
- If the dose is correct, you’ll notice a significant improvement in symptoms.
It can be a lengthy process to determine your correct dose and re-establish tolerance, but the results can be dramatic!
If you’re interested in LDI treatments, you can learn more about our LDI services and how to begin the process here.
About the Author: Dr. Seth Osgood is a Doctor of Nursing Practice, Board Certified Family Nurse Practitioner and Institute of Functional Medicine (IFM) Certified Practitioner. Dr. Osgood received his post-graduate training in Functional Medicine through the IFM and from working with Dr. Amy Myers. He has helped people from around the world improve their health utilizing a Functional Medicine approach.