There are 24 million people in the US living with an autoimmune disease.
Many of them struggle daily with debilitating symptoms or depend upon risky medications to keep them in check. This usually comes after struggling just to get a diagnosis and being told their condition will only get worse.
It doesn’t have to be this way!
This month we’re dedicating all of our articles to autoimmune issues to provide resources and hopefully some relief to those of you living with these conditions. We’ll tackle testing and diagnosis, explain the mechanism behind autoimmune attacks (and how to stop it), and share some of the newest advancements in autoimmune treatment.
If you or a loved one are looking for support in your autoimmune journey, I hope you’ll follow along!
What is Autoimmunity?
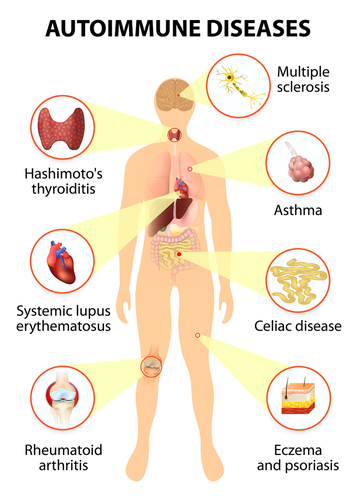
Autoimmune conditions occur when the immune system goes rogue and begins attacking your body’s own tissues.
The specific diagnosis depends on the organ being attacked. In Hashimoto’s, the thyroid is under fire, in Rheumatoid arthritis it’s the joints, in Multiple Sclerosis it’s the spinal cord, and so on.
There are three factors that cause autoimmunity, including genetics, intestinal permeability, and environmental factors.
Next week I’ll share why the attack occurs, how autoimmune disease progresses, and the principle behind stopping it.
The Challenge with Diagnosing Autoimmunity
Here’s a sobering statistic:
On average, it takes an individual with severe autoimmunity four years to get a diagnosis.
That is 1,460 days of being left in the dark having no idea of what is causing your symptoms and suffering. And remember, this is just the average. I see patients all the time who’ve spent 5, 10, 20 plus years trying to figure out why they’re sick when it has been autoimmunity the entire time.
Why does it take so many years (and often so many doctors)?
For one, there are no universal symptoms of autoimmunity. The symptoms can be vague, overlap among conditions, and vary depending upon the part of the body being attacked. However, there are strong warning signs that can lead to a clear diagnosis when coupled with a thorough history and the correct testing.
Secondly, most patients are shuttled from one specialist to another without any single provider looking at the big picture. Sometimes the forest becomes lost for the trees. This is why working with a functional medicine practitioner can be so helpful, we focus on treating the whole individual.
10 Signs You May Have an Autoimmune Disease
To help you avoid this lengthy process and gain clarity on your condition sooner, here are a few indications to pursue autoimmune testing.
- Joint pain
- Digestive issues
- Fatigue
- Swelling and redness
- Hair loss
- Brain fog
- Skin rashes
- Changes in weight
- Recurring fever
- Family history of autoimmune conditions
Testing for Autoimmune Disease
If you’re exhibiting symptoms of autoimmunity, the next step is to get a proper diagnosis through testing. This is the progression of testing we use at GrassRoots.
1. ANA Test
The first red flag that autoimmunity may be causing your symptoms is a positive antinuclear antibody or ANA test.
This test looks to identify whether or not your immune system is attacking the nuclear components of your cells. Oftentimes a positive ANA is found by doctors but gets ignored because confirmatory testing for specific diseases remains negative.
If your ANA is positive this means your immune system is attacking the nuclear components of your cells somewhere in your body. The next question should be where is it occurring?
It may not be to the point of full-blown disease yet (which is why disease-specific testing may remain negative) but if you don’t take proactive steps, there is a good chance that is where you are headed.
2. Autoimmune Profile
If you do have a positive ANA, the next thing you want to have your doctor run is a comprehensive autoimmune profile. This test can be completed by any conventional lab company and aims to detect a variety of systemic autoimmune conditions (ones that affect multiple areas of the body) like lupus, scleroderma, Sjogren’s disease, and dermatomyositis, among others.
3. Cyrex Array 5
A great test that we will often use with patients in our Adaptation Program to identify autoimmunity throughout the body is Cyrex Array 5.
This test, which is not typically run by conventional doctors, looks at autoimmune reactions in isolated organs and systems that often get overlooked in mainstream testing.
It is not uncommon to have a positive ANA with a negative conventional autoimmune profile, and have Cyrex Array 5 pop up as positive in different regions of the body.
I recently ran this test on a woman who was getting no answers from her doctors despite experiencing extreme fatigue, neurological symptoms and joint pain. Her standard autoimmune profile was negative, but lo and behold this test revealed autoimmune antibodies in her thyroid, bones, joints, and aspects of her brain and spinal cord.
As scary as these results might sound, she was relieved to know these symptoms were not in her head as she was being told by her doctors!
If you suspect autoimmunity, I highly recommend working with your provider to get the right testing and diagnosis from the start. It can save you years of suffering and prevent the disease from progressing unchecked!
About the Author: Dr. Seth Osgood is a Doctor of Nursing Practice and Institute of Functional Medicine (IFM) Certified Practitioner. Dr. Osgood received his post-graduate training in Functional Medicine through the IFM and from working with Dr. Amy Myers. He has helped people from around the world improve their health utilizing a Functional Medicine approach.
Want to work with Dr. Osgood and the GrassRoots team? Check out our Adaptation Program and book your free discovery call to find out if you’re the right fit.